What Is Osteomyelitis?
Osteomyelitis is a bone infection that is usually caused by the action of pyogenic bacteria, which produce pus. However, it can also be produced by the tuberculosis bacillus or even fungi.
Let’s see more below.
Types and causes of osteomyelitis
We can distinguish between acute and chronic osteomyelitis. The acute is the one that evolves in less than two weeks. While the chronic is the one that evolves in more than four weeks or that does not respond to antibiotic treatment. In that case, surgery would be required for healing.
In general, bone is a structure resistant to infection. However, microorganisms can enter bone through a close focus, blood, or a penetrating wound.
When talking about the causes of osteomyelitis, we can distinguish between the causes of acute and chronic osteomyelitis.
Acute osteomyelitis
The main cause of acute osteomyelitis is the spread of an infection to another organ through the blood. Although the origin of the initial infection is often unknown, the focus may be on:
- A urine infection.
- A dental infection
- Contaminated catheters.
This type of osteomyelitis occurs mostly in people under the age of 15 or over the age of 50. It also occurs frequently in patients with chronic diseases, such as cirrhosis or diabetes. On the other hand, it is associated with injection drug use.
The bacteria that most produce this type of osteomyelitis are gram positive cocci. However, it can also be caused by the tuberculosis bacteria or gram-negative bacilli.
Chronic osteomyelitis
This type of osteomyelitis is suffered mainly by adults, and is associated with:
- Surgical interventions.
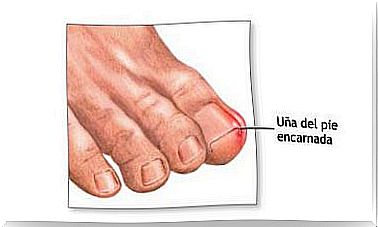
- Due to the proximity to an infectious focus.
- Trauma, mostly due to open fractures.
- Peripheral vascular pathologies, for example, the diabetic foot.
In addition, the microorganisms that can cause this infection are:
- Ischemia.
- Great positive bacteria.
- Pseudomonas in the diabetic foot.
- Open fractures with dirty wounds.
- Anaerobic bacteria present in bites.
- Certain streptococci, in the presence of a joint prosthesis.
Symptoms
The symptoms of acute osteomyelitis can be highly variable. These depend largely on how acute the infection is, the responsible microorganism, and the location of the affected bones.
In addition, it will also depend on the underlying diseases that the patient has. The most common is that the affected area appears:
- Soft tissue swelling.
- The affected area presents severe pain.
- There is a limitation of the mobility of the affected area.
Sometimes cellulitis can be associated with osteomyelitis, since it is an inflammation of the subcutaneous cell tissue and the skin. As general symptoms:
- General discomfort.
- Fever associated with chills.
- It may be the case of weight loss.
As for chronic osteomyelitis, the fever may be low or not even occur. On the other hand, local symptoms: pain, swelling and redness may be less visible at first.
Occasionally, fistulas can form where purulent discharge drains. Also, if the affected part is the spine, an epidural abscess can occur. In the most serious cases, the spinal cord can be compressed and its inflammation can occur.
Less commonly, in more severe cases , the infection can spread to areas adjacent to the spine. This would form a paravertebral abscess or in the psoas muscle.
Diagnosis
It is very important to diagnose acute osteomyelitis in a timely manner. This is because proper antibiotic treatment can prevent bone necrosis and the disease from becoming chronic. Some tests include:
- Blood cultures : This is a laboratory test to check for bacteria or other microorganisms in the blood.
- Bone biopsy : This is a test in which a piece of bone or bone marrow is removed.
- Bone scan : an imaging test used to diagnose bone diseases.
- Bone X-ray : This is an imaging test to examine the bones.
- Complete blood count (CBC) : This test measures the number of red blood cells, white blood cells, the total amount of hemoglobin in the blood, and the fraction of the blood made up of red blood cells (hematocrit).
Treatment of osteomillitis
The goal of treatment is to stop the infection, as well as to reduce possible damage to the bone and surrounding tissues. To do this, antibiotics are given to kill the bacteria causing the infection.
Keep in mind that you can receive more than one antibiotic at the same time. In addition, antibiotics are usually taken between 4 and 6 weeks, often being administered intravenously at first, followed by a subsequent switch to oral antibiotics.
This antibiotic treatment may be sufficient in the case of acute osteomyelitis. However, in chronic cases, it may be necessary to resort to surgery to clear the focus of the infection.